1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
SYMPTOMATOLOGY:
10 yrs ago- Episode of paralysis of both upper and lower limbs(right & left)
1 year ago- Right and left paresis due to hypokalemia
8 months ago-Swelling over the legs(bilateral)- Developed bilateral pedal edema which is gradually progressing and it is present both in sitting and standing position and relieved on taking medication.
7 months- Blood infection
2 months ago- Treatment for neck pain- went to hospital
6 days ago- Pain along her left upper limb associated with tingling and numbness- radiating along the left upper limb which is dragging in nature, aggravated during palpitations and relieved by taking medication for palpitations.
5 days ago-
she could feel her own heartbeat since 5 days and it is more rapid since night before admission(16/05/2021)- Palpitations: which are sudden in onset, more during night time and aggregated by lifting weights, speaking continuously and it is relieved by drinking more water, medication.
Chest pain-associated with chest heaviness.
Difficulty in breathing- dyspnea during palpitations (NYHA-CLASS-3).
Also has generalized body weakness(No idea of onset)
ANATOMICAL LOCALIZATION:HEART, SKELETAL MUSCLE AND CERVICAL SPINE
ETIOLOGY:
HYPOKALEMIA -
HYPOKALEMIA CAUSINS PALPITATIONS-
The flow of potassium in and out of heart cells helps regulate your heartbeat. Low blood potassium levels can alter this flow, resulting in heart palpitations ( 14 ). In addition, heart palpitations may be a sign of arrhythmia, or an irregular heartbeat, which is also linked to potassium deficiency.
HYPOKALEMIA PARALYSIS:
The altered channels are "leaky," allowing ions to flow slowly but continually into muscle cells, which reduces the ability of skeletal muscles to contract. Because muscle contraction is needed for movement, a disruption in normal ion transport leads to episodes of severe muscle weakness or paralysis.
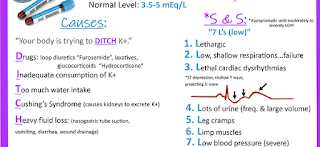
2) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
- The most common cause is excess loss from the kidneys or gastrointestinal tract. Clinical features include muscle weakness and polyuria; cardiac hyperexcitability may occur with severe hypokalemia. Diagnosis is by serum measurement. Treatment is giving potassium and managing the cause.
- Risk factors associated with a low serum potassium levels (hypokalemia) include female gender, intake of medication (diuretics), heart failure, hypertension, low body mass index (BMI), eating disorder, alcoholism, diarrhea, Cushing's syndrome.
- Hypokalemic periodic paralysis is a condition that causes episodes of extreme muscle weakness typically beginning in childhood or adolescence. Most often, these episodes involve a temporary inability to move muscles in the arms and legs. Attacks cause severe weakness or paralysis that usually lasts from hours to days.
- Hypokalemic paralysis may be caused by a short-term shift of potassium into cells, seen in hypokalemic periodic paralysis (caused by familial periodic paralysis or thyrotoxic periodic paralysis), or a larger deficit of potassium as a result of severe renal or gastrointestinal potassium loss.
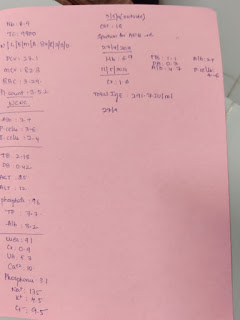
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
ECG changes include flattening and inversion of T waves in mild hypokalemia, followed by Q-T interval prolongation, visible U wave and mild ST depression in more severe hypokalemia. Severe hypokalemia can also result in arrhythmias such as Torsades de points and ventricular tachycardia.
5th CASE:
55years old patient with seizures.
Questions:
1. Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
Seizures after stroke:
You’re more likely to have a seizure if you had a hemorrhagic stroke (bleed on the brain). Seizures can also be more likely if you had a severe stroke, or a stroke in the cerebral cortex, the large outer layer of the brain where vital functions like movement, thinking, vision and emotion take place.
Some people will have repeated seizures, and be diagnosed with epilepsy. The chances of this happening may depend on where the stroke happens in the brain and the size of the stroke.
Pathogenesis:
There are several causes for early onset seizures after ischemic strokes. An increase in intracellular Ca2+ and Na+ with a resultant lower threshold for depolarization, glutamate excitotoxicity, hypoxia, metabolic dysfunction, global hypo perfusion and hyper perfusion injury ,(particularly after carotid end arterectomy) have all been postulated as putative neurofunctional etiologies. Seizures after hemorrhagic strokes are thought to be attributable to irritation caused by products of blood metabolism. The exact pathophysiology is unclear, but an associated ischemic area secondary to hemorrhage is thought to play a part. Late onset seizures are associated with the persistent changes in neuronal excitability and gliotic scarring is most probably the underlying cause. Hemosiderin deposits are thought to cause irritability after a hemorrhagic stroke.14 In childhood, post‐stroke seizures can occur as part of perinatal birth trauma.
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
Normally the “consciousness system”—a specialized set of cortical-subcortical structures—maintains alertness, attention and awareness. Diverse seizure types including absence, generalized tonic-clonic and complex partial seizures converge on the same set of anatomical structures through different mechanisms to disrupt consciousness.
6th CASE:
A 48 year old male with seizures and altered sensorium
Questions:
1) What could have been the reason for this patient to develop ataxia in the past 1 year?
The reason for patient to develop ataxia in past one year is ALCOHOL:
Damage from alcohol is a common cause of cerebellar ataxia. In patients with alcohol related ataxia, the symptoms affect gait (walking) and lower limbs more than arms and speech. It can also cause associated signs of peripheral neuropathy. Peripheral neuropathy is damage to the body's peripheral nervous system.
|
Peripheral neuropathy is damage to the body's peripheral nervous
system. This can cause muscle weakness, numbness and tingling,
burning pain and a loss of coordination. This peripheral neuropathy, can
contribute to the ataxia.
|
Inside the brain, alcohol directly damages certain cells within the
cerebellum and the rest of the brain, and for those people who drink
excessively over a long period of time it can cause particularly severe and
often permanent damage.
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ?
This peripheral neuropathy, can contribute to the ataxia. Inside the brain, alcohol directly damages certain cells within the cerebellum and the rest of the brain, and for those people who drink excessively over a long period of time it can cause particularly severe and often permanent damage.
|
Cerebellar ataxia is a common finding in neurological practice and has a wide variety of causes, ranging from the chronic and slowly-progressive cerebellar degenerations to the acute cerebellar lesions due to infarction, edema and hemorrhage, configuring a true neurological emergency.
- Excessive drinking isn't good for anyone, but it is especially dangerous for people with bleeding disorders, potentially leading to falls and brain bleeds. Alcohol use is also known to raise blood pressure, and high blood pressure is already associated with blood disorders.
- Liver damage due to too much alcohol can stop the liver from making substances that help your blood to clot. This can increase your risk of having a stroke caused by bleeding in your brain.
Our results showed that heavy drinkers were about 1.6 times more likely to suffer from intracerebral hemorrhage and 1.8 times more likely to suffer from subarachnoid hemorrhage. The association between heavy alcohol consumption and these two types of stroke was stronger than that for ischemic stroke.
7th CASE:
A 30 YR OLD MALE PATIENT WITH WEAKNESS OF RIGHT UPPER LIMB AND LOWERLIMB
Questions:
1.Does the patient's history of road traffic accident have any role in his present condition?
Main injurie in road traffic accident: Whiplash injuries
Whiplash injuries have the potential to cause damage to the main artery (the carotid artery) which supplies blood to the brain, resulting in a stroke. Initially a minor injury – such as whiplash – may not appear to have a life-changing impact, but sadly it can develop into a stroke several weeks later.
Car accidents can cause a number of injuries ranging from head wounds to broken bones and bruises. Generally, car accident trauma is not linked to strokes because oftentimes the stroke does not occur right away. Due to this, strokes that happen weeks after a car accident are disregarded.
2.What are warning signs of CVA?
Warning Signs
- Numbness or weakness in your face, arm, or leg, especially on one side.
- Confusion or trouble understanding other people.
- Difficulty speaking.
- Trouble seeing with one or both eyes.
- Problems walking or staying balanced or coordinated.
- Dizziness.
- Severe headache that comes on for no reason.
3.What is the drug rationale in CVA?
1.Injection Mannitol:
The role of mannitol therapy in acute stroke is controversial. Because of its osmotic effect, mannitol is assumed to decrease cerebral edema. Mannitol might improve cerebral perfusion by decreasing viscosity, and as a free-radical scavenger, it might act as a neuroprotectant.
2.TAB Ecosprin:
Taking an aspirin for an ischemic stroke can prevent further clot formation. “More than 85 percent of all strokes are ischemic,” . “Aspirin is helpful if taken within the first 48 hours of an ischemic stroke.”
3.TAB ATORVAS:
In patients with recent stroke or TIA and without known coronary heart disease, 80 mg of atorvastatin per day reduced the overall incidence of strokes and of cardiovascular events, despite a small increase in the incidence of hemorrhagic stroke.
4.BP/PR/TEMP/SP02 MONITORING:
Several aspects of physiology, notably blood pressure, body temperature, blood glucose, and blood oxygen saturation, may be altered after an ischemic stroke and intracerebral hemorrhage. Generally, blood pressure and temperature rise acutely after a stroke, before returning to normal.
5.RT FEEDS-100ml milk with protein powder:
Enteral feeding tubes, a nasogastric tube (NGT) or percutaneous endoscopic gastrostomy (PEG), are commonly used to provide nutrition, hydration and essential medications to stroke patients who cannot swallow.
4. Does alcohol has any role in his attack?
HE IS OCCASIONAL ALCOHOLIC(500ml of alcohol (whiskey) once in a week). HE DIDNT STOP ALCOHOL after accident.
BUT before fall, previous night he dint drink alcohol.
SO, ALCOHOL HAS NO ROLE IN HIS ATTACK.
If you have had a hemorrhagic stroke, you must not drink alcohol for at least three weeks after your stroke. Drinking too much alcohol contributes to a number of risk factors for stroke, including high blood pressure. Alcohol can interfere with the medicine you take to reduce stroke risk.
5.Does his lipid profile has any role for his attack?
IN THIS PATIENT WE CAN SEE DECREASE IN HDL
HDL (high-density lipoprotein), or “good” cholesterol, absorbs cholesterol and carries it back to the liver. The liver then flushes it from the body. High levels of HDL cholesterol can lower your risk for heart disease and stroke.
In one study of the very old (aged ≥85 years) low serum HDL-C was associated with an increased risk of stroke, cardiovascular disease, and mortality whereas LDL-C and total cholesterol had no association.
Findings revealed a significant relation between lipid profile and the occurrence of the ischemic stroke. LDL was considered as a predictor of hemorrhagic stroke, as well. It also reported that increased cholesterol and LDL levels are associated with higher risk of developing ischemic stroke.
8th CASE:
A 50 YEAR OLD PATIENT WITH CERVICAL MYELOPATHY
Questions:
1)What is myelopathy hand ?
There is loss of power of adduction and extension of the ulnar two or three fingers and an inability to grip and release rapidly with these fingers. These changes have been termed "myelopathy hand" and appear to be due to pyramidal tract involvement.
2)What is finger escape ?
Wartenberg's sign is a neurological sign consisting of involuntary abduction of the fifth (little) finger, caused by unopposed action of the extensor digiti minimi. This finding of weak finger adduction in cervical myelopathy is also called the "finger escape sign".
3)What is Hoffman’s reflex?
Hoffmann sign was elicited by flicking the nail of the middle finger. Any flexion of the ipsilateral thumb and/or index finger was considered positive. All imaging studies were reviewed for spinal cord compression.
Hoffman's sign or reflex is a test that doctors use to examine the reflexes of the upper extremities. This test is a quick, equipment-free way to test for the possible existence of spinal cord compression from a lesion on the spinal cord or another underlying nerve condition.
9th CASE:
A 17 year old female with seizures
Questions:
1) What can be the cause of her condition ?
According to MRI cortical vein thrombosis might be the cause of her seizures.
2) What are the risk factors for cortical vein thrombosis?
Infections:
Meningitis, otitis, mastoiditis
Prothrombotic states:
Pregnancy, puerperium, antithrombin deficiency proteins and protein s deficiency, Hormone replacement therapy.
Mechanical:
Head trauma, lumbar puncture
Inflammatory:
SLE, sarcoidosis, Inflammatory bowel disease.
Malignancy.
Dehydration
Nephrotic syndrome
Drugs:
Oral contraceptives, steroids, Inhibitors of angiogenesis
Chemotherapy: Cyclosporine and l asparaginase
Hematological:
Myeloproliferative Malignancies
Primary and secondary polycythemia
Intracranial :
Dural fistula,
venous anomalies
Vasculitis:
Bechet's disease
Wegener's granulomatosis
3)There was seizure free period in between but again sudden episode of GTCS why? resolved spontaneously why?
Seizures are resolved and seizure free period got achieved after medical intervention but sudden episode of seizure was may be due to any persistence of excitable foci by abnormal firing of neurons.
4) What drug was used in suspicion of cortical venous sinus thrombosis?
Anticoagulants are used for the prevention of harmful blood clots.
Clexane ( enoxaparin) low molecular weight heparin binds and potentiates antithrombin three a serine protease Inhibitor to form complex and irreversibly inactivates factor xa.
CARDIOLOGY:
10th CASE:
A 78YEAR OLD MALE WITH SHORTNESS OF BREATH, CHEST PAIN, B/L
PEDAL EDEMA AND FACIAL PUFFINESS
Questions:
1.What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
Heart failure with preserved ejection fraction (HFpEF) – also referred to as diastolic heart failure. The heart muscle contracts normally but the ventricles do not relax as they should during ventricular filling (or when the ventricles relax).
Heart failure with reduced ejection fraction (HFrEF) happens when the left side of your heart doesn't pump blood out to the body as well as normal. It's sometimes called systolic heart failure.
2.Why haven't we done pericardiocentesis in this patient?
Pericardiocentesis is the most useful therapeutic procedure for the early management or diagnosis of large, symptomatic pericardial effusion and cardiac tamponade.
Pericardiocentesis is not done because:
The effusion was self healing. It reduced from 2.07cm to 1.4mm
The effusion is small sac over 1cm
Cardiac tamponade is not found
3.What are the risk factors for development of heart failure in the patient?
Diabetes. Having diabetes increases your risk of high blood pressure and coronary artery disease.
Alcohol use. Drinking too much alcohol can weaken heart muscle and lead to heart failure.
Tobacco use. Using tobacco can increase your risk of heart failure
High blood pressure. Your heart works harder than it has to if your blood pressure is high.
AV BLOCK
Pericardial effusion if worsen
If use any medications which may cause heart failure
Atrial premature complexes
4.What could be the cause for hypotension in this patient?
Patient is on medication like lasix (Diuretics) from few days.
He is also anemic, So this may cause hypotension even he is hypertensive patient
Pericardial effusion may not be reason because it is in moderate condition which nay not cause hypotension and also no cardiac tamponade is found.
11th CASE:
A 73 YEAR OLD MALE PATIENT WITH PEDAL EDEMA, SHORTNESS OF BREATH AND
DECREASED URINE OUTPUT
Questions:
1.What are the possible causes for heart failure in this patient?
- Diabetes mellitus: Diabetic patients have an increased risk of developing heart failure because of the abnormal cardiac handling of glucose and free fatty acids (FFAs), and because of the effect of the metabolic derangements of diabetes on the cardiovascular system
- Hyper tension: High blood pressure forces your heart to work harder to pump blood to the rest of your body. This causes part of your heart (left ventricle) to thicken. A thickened left ventricle increases your risk of heart attack, heart failure and sudden cardiac death. Heart failure.
- CKD stage 4: Damaged kidneys may release too much of an enzyme called renin, which helps to control blood pressure. This increases your risk for heart attack, congestive heart failure and stroke.
- Chronic alcoholic: Long-term alcohol abuse weakens and thins the heart muscle, affecting its ability to pump blood. When your heart can't pump blood efficiently, the lack of blood flow disrupts all your body's major functions. This can lead to heart failure and other life-threatening health problems
- Atrial fibrillation: By not getting enough oxygen to the body, afib can lead to heart and valve diseases, sleep apnea, and chronic fatigue. In addition, atrial fibrillation can lead to two potentially life-threatening conditions, congestive heart failure and stroke
- COVID-19
2.what is the reason for anemia in this case?
- Red blood cells are made by the bone marrow. To get the marrow to make red blood cells, the kidneys make a hormone called erythropoietin, or EPO. When the kidneys are damaged, they may not make enough EPO. Without enough EPO, the bone marrow does not make enough red blood cells, and you have anemia.
- Red blood cells are constantly turned over by the body, so too much red blood cell destruction can also lead to anemia. While alcohol and anemia are generally not thought to be related, drinking too much alcohol can lead to anemia.
- Diabetes is the single most common cause of end-stage renal disease (1) and therefore the most common cause of renal anemia. In addition, anemia may be more common in diabetes (2) and develop earlier than in patients with renal impairment from other causes.
3.What is the reason for blebs and non healing ulcer in the legs of this patient?
Leg ulcers are debilitating and greatly reduce patients' quality of life. The common causes are venous disease, arterial disease, and neuropathy. Less common causes are metabolic disorders, hematological disorders, and infective diseases.
- Uncontrolled diabetes mellitus(Diabetic neuropathy)- Circulation of blood at the wound site is critical for wound healing. As a result of narrowed blood vessels, diabetic wound healing is impaired because less oxygen can reach the wound and the tissues do not heal as quickly.
- Kidney failure
- Pressure due to any shoes, etc.
- Trauma
- Hypertension
4. What sequence of stages of diabetes has been noted in this patient?
According to case details he had crossed all stages of diabetes.
stage 1: defined as DCBD insulin resistance;
stage 2: defined as DCBD prediabetes;
stage 3: defined as DCBD type 2 diabetes;
stage 4: defined as DCBD vascular complications, including retinopathy, nephropathy or neuropathy, and/or type 2 diabetes-related microvascular events.
12th CASE:
A-Fib and Biatrial Thrombus in a 52yr old Male
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
SYMPTOMATOLOGY:
10 years ago: SURGERY FOR INGUINAL HERNIA
3 years ago: H/O NSAID ABUSE + FACIAL PUFFINESS(ON&OFF)
2 years ago: FACIAL PUFFINESS
1 year ago: SOB(GRADE-2)
13/05/2021: SOB(GRADE-2) TO SOB(GRADE-4)+DECREASE IN URINE OUTPUT+CONSTIPATION
15/05/2021: ANURIA
ANATOMICAL LOCALIZATION: Blood vessels and Atrium
ETIOLOGY: HYPERTENSION
- Blood vessels damaged by high blood pressure can narrow, rupture or leak. High blood pressure can also cause blood clots to form in the arteries leading to your brain, blocking blood flow and potentially causing a stroke.
- High blood pressure forces your heart to pump harder and harder. When your heart is pushed to the limit for too long, the muscle doesn't get stronger – it gets thicker and stiffer. Electrical signals can't move as easily through a less flexible, enlarged heart muscle, and that could lead to AFib.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
DOBUTAMINE:
MOA-Dobutamine is a synthetic catecholamine that acts on alpha-1, beta-1 and beta-2 adrenergic receptors. In the heart, the stimulation of these receptors produces a relatively strong, additive inotropic effect and a relatively weak chronotropic effect.
Indications: Cardiogenic shock, Reversible heart failure.
Efficacy: Dobutamine infusion significantly increased cardiac index, stroke index, and pulmonary capillary wedge pressure, and it decreased systemic vascular resistance. The drug appears more efficacious in treating cardiogenic shock than septic shock.
DIGOXIN:
MOA and Indications- It has two principal mechanisms of action which are selectively employed depending on the indication:
- Positive Ionotropic: It increases the force of contraction of the heart by reversibly inhibiting the activity of the myocardial Na-K ATPase pump, an enzyme that controls the movement of ions into the heart. Digoxin induces an increase in intracellular sodium that will drive an influx of calcium in the heart and cause an increase in contractility. Cardiac output increases with a subsequent decrease in ventricular filling pressures.
- AV Node Inhibition: Digoxin has vagomimetic effects on the AV node. By stimulating the parasympathetic nervous system, it slows electrical conduction in the atrioventricular node, therefore, decreases the heart rate. The rise in calcium levels leads to prolongation of phase 4, and phase 0 of the cardiac action potential thus increases the refractory period of the AV node. Slower conduction through the AV node carries a decreased ventricular response.
Efficacy-Across all study types, digoxin led to a small but significant reduction in all cause hospital admission (risk ratio 0.92, 0.89 to 0.95; P<0.001; n=29 525). Conclusions Digoxin is associated with a neutral effect on mortality in randomised trials and a lower rate of admissions to hospital across all study types.
CARDIVAS:
MOA- Tablet is an alpha and beta blocker. It works by slowing down the heart rate and relaxing blood vessels which makes the heart more efficient at pumping blood around the body.
Indications- Medicine used to treat high blood pressure, heart-related chest pain (angina), and heart failure.
CARVIDILOL:
MOA- Carvedilol reversibly binds to beta adrenergic receptors on cardiac myocytes. Inhibition of these receptors prevents a response to the sympathetic nervous system, leading to decreased heart rate and contractility.
Indications- Carvedilol is a non-selective adrenergic blocker indicated for the chronic therapy of heart failure with reduced ejection fraction (HFrEF), hypertension, and left ventricular dysfunction following myocardial infarction (MI) in clinically stable patients.
Efficacy- Carvedilol is a nonselective vasodilating β-adrenergic blocker with α1 adrenergic-blocking activities28,29 with established efficacy in decreasing mortality and morbidity in patients with mild to severe chronic HF with systolic left ventricular dysfunction (LVD).
INJ. HAI S/C:
MOA- Regulates glucose metabolism
Hypoglycemia symptoms explained
Watch for any bleeding manifestations like Petechiae, bleeding gums
APTT and INR are ordered on a regular basis when a person is taking the anticoagulant drug warfarin to make sure that the drug is producing the desired effect.
3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
| Type 4 | Chronic renocardiac syndrome | Chronic kidney injury leads to chronic cardiac dysfunction(eg; coronary disease, heart failure or arryhthmia |
4) What are the risk factors for atherosclerosis in this patient?
HYPERTENSION:
People with high blood pressure are more likely to develop coronary artery disease, because high blood pressure puts added force against the artery walls. Over time, this extra pressure can damage the arteries, making them more vulnerable to the narrowing and plaque buildup associated with atherosclerosis.
5) Why was the patient asked to get those APTT, INR tests for review?
APTT and INR are ordered on a regular basis when a person is taking the drug warfarin to make sure that the drug is producing the desired effect.
Here, an INR of 3-4.5 is recommended. Warfarin should be started in conjunction with heparin or low molecular weight heparin when the diagnosis of venous thromboembolism is confirmed, although local protocols may vary in their starting doses and titration schedule.
13th CASE:
67 year old patient with acute coronary syndrome
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
SYMPTOMATOLOGY:
12 years ago- DM TYPE 2-TREATMENT-GLIMI
1 year ago- HEART BURN LIKE EPISODES-RELIEVES WITHOUT MEDICATION
7 months ago- TB CURRENTLY NEGATIVE
6 months ago- HYPERTENSION-TELMA
14/05/2021- 1/2 HR BEFORE COMING TO HOSPITAL- SOB
ANATOMICAL LOCALIZATION:BLOOD VESSELS OF HEART
ETIOLOGY: Atherosclerosis(plague or clot formation), HTN.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Tablet belongs to a group of medicines called long-acting beta-blocker. It works by blocking the effects of some chemicals on your heart and blood vessels. It slows down your heart rate and helps it to beat with less force.
Indications- Angina pectoris, Heart failure, Cardiac arrhythmias
- Percutaneous Coronary Intervention (PCI, formerly known as angioplasty with stent) is a non-surgical procedure that uses a catheter (a thin flexible tube) to place a small structure called a stent to open up blood vessels in the heart that have been narrowed by plaque buildup, a condition known as atherosclerosis.
3) What are the indications and contraindications for PCI?
Percutaneous coronary intervention (PCI), also known as coronary angioplasty, is a nonsurgical technique for treating obstructive coronary artery disease, including unstable angina, acute myocardial infarction (MI), and multi vessel coronary artery disease (CAD)
INDICATIONS:
Acute ST-elevation myocardial infarction (STEMI)Non–ST-elevation acute coronary syndrome (NSTE-ACS)Unstable angina.Stable angina.Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)High risk stress test findings. CONTRAINDICATIONS:
Intolerance for oral antiplatelet long-term.Absence of cardiac surgery backup.Hypercoagulable state.High-grade chronic kidney disease.Chronic total occlusion of SVG.An artery with a diameter of <1.5 mm.In this case a PCI was not done due to non availability of vacancies in higher centres due to the ongoing pandemic. Instead she was sent home with a prescription.
4) What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on over testing and overtreatment important to current healthcare systems?
Although PCI is generally a safe procedure , it might cause serious certain complications like
A)Bleeding
B) Blood vessel damage
C) Allergic reaction to the contrast dye used
D) Arrhythmias
E) Need for emergency coronary artery bypass grafting .
Because of all these complications it is better to avoid PCI in patients who do not require it.
Relative contraindications to PCI include
Lack of cardiac surgical support
Critical left main coronary stenosis without collateral flow from a native vessel or previous bypass graft to the left anterior descending artery
Diffusely diseased vessels without focal
stenosisA single diseased vessel providing all perfusion to the myocardium
Total occlusion of a coronary artery
Although lack of cardiac surgical support is sometimes considered an absolute contraindication to PCI, many experts advocate that when revascularization is required urgently in STEMI, experienced operators in approved catheterization laboratories should proceed with PCI even if surgical backup is not available.
Although bypass is typically preferred for patients with critical left main coronary stenosis without collateral flow from either a native vessel or previous bypass graft, PCI is increasingly being used in this scenario in selected patients.
- OVER TESTING AND OVER TRAETMENT HAVE BECOME COMMMIN IN TODAY’S MEDICAL PRACTICE.
- Research on over testing and overtreatment is important as they are more harmful than useful.
- Harms to patients
- . Performing screening tests in patients with who at low risk for the disease which is being screened.
- For example: Breast Cancer Screenings Can Cause More Harm Than Good in Women Who Are at Low Risk. A harmless lump or bump could incorrectly come up as cancer during routine breast screenings. This means that some women undergo surgery, chemotherapy or radiation for cancer that was never there in the first place.
- Overuse of imaging techniques such as X- RAYS AND CT SCANS as a part of routine investigations.
- Overuse of imaging can lead to a diagnosis of a condition that would have otherwise remained irrelevant - OVERDIAGNOSIS.
- Also the adverse effects due to this are more when compared to the benefits.
- Over diagnosis through over testing can psychologically harm the patient.
- Hospitalizations for those with chronic conditions who could be treated as outpatients[ can lead to economic burden and a feeling of isolation.
- Harms to health care systems
- The use of expensive technologies and machineries are causing burden on health care systems.
The potential consequences of overuse may be significant and include such harms as the psychological and behavioral effects of disease labelling, physical harms and side effects of unnecessary tests or treatments, the 'burden of treatment' negatively affecting quality of life.- Overtreatment following over diagnosis can lead to clinically important consequences, including death from the side effects of treatment—for example, sepsis in a patient undergoing chemotherapy for treatment of an over diagnosed cancer.
14th CASE:
CASE DISCUSSION ON
ACUTE MYOCARDIAL INFARCTION
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
SYMPTOMATOLOGY:
Long time ago- HTN AND DM
3days ago of admission- CHEST PAIN(INSIDIOUS,GRADUAL, DRAGGING TYPE)
14/05/2021- MORNING OF ADMISSION-GIDDINESS+PROFUSE SWEATING
ANATOMICAL LOCALIZATION: BLOOD VESSELS OF HEART
ETIOLOGY: Atherosclerosis
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ASPIRIN:
MOA- Aspirin acts as an acetylating agent where an acetyl group is covalently attached to a serine residue in the active site of the COX enzyme. This makes aspirin different from other NSAIDs (such as diclofenac and ibuprofen), which are reversible inhibitors.
Indication-
Angina pectoris.
- Angina pectoris prophylaxis.
- Ankylosing spondylitis.
- Cardiovascular risk reduction.
- Colorectal cancer.
- Fever.
- Ischemic stroke.
- Ischemic stroke: Prophylaxis
ATORVAS:
MOA- Atorvastatin competitively inhibits 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase. By preventing the conversion of HMG-CoA to mevalonate, statin medications decrease cholesterol production in the liver.
Indication-
- Reduce the risk of non-fatal myocardial infarction.
- Reduce the risk of fatal and non-fatal stroke.
- Reduce the risk for revascularization procedures.
- Reduce the risk of hospitalization for CHF.
- Reduce the risk of angina.
3) Did the secondary PTCA do any good to the patient or was it unnecessary?
Yes, it does good to the patient.
15th CASE:
CARDIOGENIC SHOCK CASE
Questions:
1. How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
Because of the fluid loss occurred to the patient
there is decreased preload- so, SOB occurred due to decreased CO
IV fluids administered- there is increased preload- SOB decreased due to better of cardiac output.
2. What is the rationale of using torsemide in this patient?
Torsemide used to relieve abdominal distension.
3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
IT IS THE TREATMENT FOR UTI
Rationale- Used for any bacterial infection.
GASTROENTEROLOGY (& PULMONOLOGY):
16th CASE:
A
33 YEAR OLD MAN WITH PANCREATITIS, PSEUDOCYST AND LEFT BRONCHO-PLEURAL FISTULA
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
SYMPTOMATOLOGY:
5 years back-1st episode of pain abdomen and vomiting
Stopped taking alcohol for 3 years
1 year back 5 to 6 episodes of pain abdomen and vomiting after starting to drink alcohol again
20 days back increased consumption of toddy intake
Since 1 week pain abdomen and vomiting
Since 4 days fever constipation and burning micturition
ANATOMICAL LOCALIZATION:
PANCREAS AND LUNG
ETIOLOGY: Alcohol and its metabolites produce changes in the acinar cells, which may promote premature intracellular digestive enzyme activation thereby predisposing the gland to autodigestive injury. Pancreatic stellate cells (PSCs) are activated directly by alcohol and its metabolites and also by cytokines and growth factors released during alcohol-induced pancreatic necroinflammation. Activated PSCs are the key cells responsible for producing the fibrosis of alcoholic chronic pancreatitis.
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
1) ING. MEROPENAM ; TID for 7 days
* Meropenem ( broad spectrum Carbapenem ) an antibiotic.
2) ING. METROGYL 500 mg IV TID for 5 days
* inj. Metrogyl has METRONIDAZOLE
( Nitroimidazole drug ) an antibiotic
3) ING. AMIKACIN 500 mg IV BD for 5days
* It is an Aminoglycoside antibiotic
## Here all three of these (Inj. Meropenem, Inj. Metrogyl, Inj. Amikacin ) are used as antibiotics to control infection and ; to prevent septic complications of acute pancreatitis.
4) TPN ( Total Parenteral Nutrition )
* Method of feeding that by passes gastrointestinal tract
* Fluids are given to vein , it provides most of the nutrients body needs.
* TPN has proteins, carbohydrates, fats, vitamins, minerals.
5) IV NS / RL at the rate 12l ml per hour
* Given for fluid replacement ie., treat dehydration
6) ING. OCTREOTIDE 100 mg SC , BD
* It is a Somatostatin long acting analogue.
* It is used here to decrease exocrine secretion of pancreas and it also has anti- inflammatory & cytoprotective effects.
7) ING. PANTOP 40 mg IV , OD
* Inj. Pantop has PANTOPRAZOLE ( Proton Pump Inhibitor) used for its anti pancreatic secretory effect.
8) ING. THIAMINE 100 mg in 100 ml NS IV , TID
* It is B1 supplement.
* It is given here because; due to long fasting & TPN usage , body may develop B1 deficiency
* Wernicke encephalopathy secondary to B1 deficiency may be caused... so a prophylactic B1 supplementation is necessary.
9) ING. TRAMADOL in 100 ml NS IV , OD
* It is an opioid analgesic, given to relive pain
- Me as a treating physician will follow same approach followed by the treating team
- And I would like to follow up patient with- CYSTOGASTROSTOMY & MRCP
17th CASE:
CASE DISCUSSION ON 25 YEAR OLD MALE WITH EPIGASTRIC PAIN
Questions:
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
The cause of dyspnea might be PLEURAL EFFUSION
Presence of pleural effusion is currently considered an indication of severe pancreatitis and not just a marker of the disease[24]. Pancreatic ascites and pleural effusion are rare complications of both chronic and acute pancreatitis, and are associated with a mortality rate of 20% to 30%
2) Name possible reasons why the patient has developed a state of hyperglycemia.
This hyperglycemia could thus be the result of a hyperglucagonemia secondary to stress
The result of decreased synthesis and release of insulin secondary to the damage of pancreatic β-cells
Elevated levels of catecholamines and cortisol
Infection and sepsis
Alcohol abuse
Denovo type 2 DM
3) What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
Conversely, about 95% of patients with acute cholecystitis have cholelithiasis. When a stone becomes impacted in the cystic duct and persistently obstructs it, acute inflammation results. Bile stasis triggers release of liver enzymes e.g., serum 5 NT, ALP, AST, ALT along with serum bilirubin level.
The biochemical markers for chronic alcohol consumption that have been most commonly studied are serum GGT, AST, ALT, mean corpuscular volume (MCV) and carbohydrate-deficient transferrin (CDT). An AST to ALT ratio over 2 is highly suggestive of ALD
4) What is the line of treatment in this patient?
Plan of action and Treatment:
Investigations:
✓ 24 hour urinary protein
✓ Fasting and Post prandial Blood glucose
✓ HbA1c
✓ USG guided pleural tapping
Treatment:
• IVF: 125 mL/hr
• Inj PAN 40mg i.v OD
• Inj ZOFER 4mg i.v sos
• Inj Tramadol 1 amp in 100 mL NS, i.v sos
• Tab Dolo 650mg sos
• GRBS charting 6th hourly
• BP charting 8th hourly
18th CASE:
A 45 year old Female
patient with Fever, Pain abdomen, Decreased Urine output and Abdominal
distension
Questions:
1) what is the most probable diagnosis in this patient?
Differential Diagnosis:
· Ruptured Liver Abscess.
· Organized collection secondary to Hollow viscous Perforation.
· Organized Intraperitoneal Hematoma.
· Free fluid with internal echoes in Bilateral in the Sub diaphragmatic space.
· Grade 3 RPD of right Kidney
The most probably diagnosis is there is abdominal hemorrhage. This will give reasoning to the abdominal distention, and the blood which is aspirated.
2) What was the cause of her death?
After leaving the hospital, the patient went to Hyderabad and underwent an emergency laparotomy surgery. The patient passed away the next day. Cause of her death can be due to complications of laparotomy surgery such as, hemorrhage (bleeding), infection, or damage to internal organs.
3) Does her NSAID abuse have something to do with her condition? How?
NSAID-induced renal dysfunction has a wide spectrum of negative effects, including decreased glomerular perfusion, decreased glomerular filtration rate, and acute renal failure. Chronic NSAIDs use has also been related to hepatotoxicity. While the major adverse effects of NSAIDs such as gastrointestinal mucosa injury are well known, NSAIDs have also been associated with hepatic side effects ranging from asymptomatic elevations in serum aminotransferase levels and hepatitis with jaundice to fulminant liver failure and death.
NEPHROLOGY (& UROLOGY):
19th CASE:
Post TURP with non oliguric ATN
Questions:
1. What could be the reason for his SOB ?
His sob was is due to
Acidosis which was caused by Diuretics.
Hypotension nd Bradycardia which are complications of the turp. The blood loss which is more because the size of the gland is 60grams.....all these factors hypovolemia nd Bradycardia all these culminate nd results in SOB
2. Why does he have intermittent episodes of drowsiness ?
Hyponatremia was the cause for his drowsiness.
Increased levels of creatinine in the body...
When the creatinine quantity decreased to normal level the patient the patient become allright.
But again when the creatinine levels raises the patient becomes drowsy.
3. Why did he complaint of fleshy mass like passage in his urine?
patient feels thick urine coming out of his body...the reason behind is the patient had urosepsis.....the culture and sensitivity showed the E.coli infection...it is the most common cause of UTI....because these infection many pus cells has formed...and these pus cells increase the cloudiness of the urine ..so the patient feels fleshy mass like urine..
4. What are the complications of TURP that he may have had?
Difficulty micturition
Electrolyte imbalances
Infection
INTRA-OPERATIVE COMPLICATIONS
1-Hypotension
2-TURP syndrome
3-Haemorrhage
4-Perforation of bladder/prostatic capsule
5-Hypothermia
6-Bacteremia and sepsis
7-Complications of positioning
8-Erection
20th CASE:
An Eight year old with Frequent Urination
Questions:
1.Why is the child excessively hyperactive without much of social etiquettes ?
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by inattention, or excessive activity and impulsivity, which are otherwise not appropriate for a person's age
For a diagnosis, the symptoms have to be present for more than six months, and cause problems in at least two settings (such as school, home, work, or recreational activities).
2. Why doesn't the child have the excessive urge of urination at night time ?
Since the child doesn’t have excessive urge of urination at night but at day there might be a psychiatry related condition
1. Psychosomatic disorder
2. Undiagnosed anxiety disorder
3. How would you want to manage the patient to relieve him of his symptoms?
Bacterial kidney infection, the typical course of treatment is antibiotic and painkiller therapy.
If the cause is an overactive bladder, a medication known as an anticholinergic may be used. These prevent abnormal involuntary detrusor muscle contractions from occurring in the wall of the bladder
To treat attention deficit hyperactivity disorder:
For children 6 years of age and older, the recommendations include medication and behavior therapy together — parent training in behavior management for children up to age 12 and other types of behavior therapy and training for adolescents. Schools can be part of the treatment as well.
Methylphenidate A stimulant and a medication used to treat Attention Deficit Hyperactivity Disorder. It can make you feel very ‘up’, awake, excited, alert and energized, but they can also make you feel agitated and aggressive. They may also stop you from feeling hungry.
Amphetamine belongs to a class of drugs known as stimulants. It can help increase your ability to pay attention, stay focused on an activity, and control behavior problems. It may also help you to organize your tasks and improve listening skills.
INFECTIOUS DISEASE (HI virus, Mycobacteria, Gastroenterology, Pulmonology):
21st CASE:
A 40 YEAR OLD LADY WITH DYSPHAGIA, FEVER AND COUGH
Questions:
1.Which clinical history and physical findings are characteristic of tracheoesophageal fistula?
Here in this patient:
Clinical history:
Cough on taking foods and liquids which was initially non productive then associated with sputum which is white in colour and non foul smelling.
Difficult in swallowing since 2 months with solids and liquids. Patient is on RT feeding.
History of weight loss and SOB
One episode of vomiting
Fever episodes
Physical finding:
Thinly built and malnourished
Respiratory system examination: Wheeze present in bilateral mammary areas.
Neck examination: laryngeal crepitus- positive
2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
A paradoxical clinical worsening of a known condition or the appearance of a new condition after initiating antiretroviral therapy (ART) therapy in HIV-infected patients resulting from restored immunity to specific infectious or non-infectious antigens is defined as immune reconstitution inflammatory syndrome (IRIS).
Because clinical deterioration occurs during immune recovery, this phenomenon has been described as immune restoration disease (IRD), immune reconstitution syndrome (IRS), and paradoxical reactions. Given the role of the host inflammatory response in this syndrome, the term (IRIS) has been proposed and has become the most widely used and accepted term to describe the clinical entity.
Diagnostic Criteria for IRIS
Major criteria
Atypical presentation of “opportunistic infections (OI) or tumors” in patients responding to antiretroviral therapy.
Decrease in plasma HIV RNA level by at least 1 log10copies/mL.
Minor criteria
Increased blood CD4+ T-cell count after HAART.
Increase in immune response specific to the relevant pathogen, e.g. DTH response to mycobacterial antigens.
Spontaneous resolution of disease without specific antimicrobial therapy or tumor chemotherapy with continuation of antiretroviral therapy.
According to this article, and above given information this patient may have less chances of developing IRIS.
Prevention of IRIS:
The most effective prevention of IRIS would involve initiation of ART before the development of advanced immunosuppression. IRIS is uncommon in individuals who initiate antiretroviral treatment with a CD4+ T-cell count greater than 100 cells/uL.
Aggressive efforts should be made to detect asymptomatic mycobacterial or cryptococcal disease prior to the initiation of ART, especially in areas endemic for these pathogens and with CD4 T-cell counts less than 100 cells/uL.
Two prospective randomized studies are evaluating prednisone and meloxicam for the prevention of paradoxical TB IRIS.
INFECTIOUS DISEASE & HEPATOLOGY:
22nd CASE:
Questions:
1. Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors present in it ? What could be the cause in this patient ?
yes, it could be due to intake of contaminated toddy.
It was undoubtedly proven that alcoholism, mainly consuming locally prepared alcohol plays a major role as a predisposing factor for the formation of liver abscesses that is both amoebic as well as pyogenic liver abscess because of the adverse effects of alcohol over the Liver.
2. What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
According to some studies, alcoholism mainly consuming locally prepared alcohol plays a major role as a predisposing factor for the formation of liver abscesses that is both amoebic as well as pyogenic liver abscess because of the adverse effects of alcohol over the Liver. It is also proven that Alcoholism is never an etiological factor for the formation of liver abscess.
3. Is liver abscess more common in right lobe ?
Yes right lobe is involved due to its more blood supply and
The usual pattern of abscess formation is that there is leakage from the bowel in the abdomen that travels to the liver through the portal vein.
4.What are the indications for ultrasound guided aspiration of liver abscess ?
Indications for USG guided aspiration of liver abscess
1. Large abscess more than 6cms
2. Left lobe abscess
3.Caudate lobe abscess
4. Abscess which is not responding to drugs
23rd CASE:
CASE
DISCUSSION ON LIVER ABCESS
Questions:
1) Cause of liver abscess in this patient ?
Cause of liver abscess in this patient is ENTAMOEBA HISTOLYTICA.
Amebic liver abscess is the most common extra-intestinal manifestation of the protozoan, Entamoeba histolytica. The life cycle involves consumption of fecally contaminated food and water, that reaches and penetrates the small intestine to enter the mesenteric vessels and finally the liver.
2) How do you approach this patient ?
Antibiotics such as metronidazole (Flagyl) or tinidazole (Tindamax) are the usual treatment for liver abscess. A drug such as paromomycin or diloxanide must also be taken to get rid of all the ameba in the intestine and to prevent the disease from coming back.
3) Why do we treat here ; both amoebic and pyogenic liver abscess?
Amebic abscesses are more common in areas where Entamoeba histolytica is endemic, whereas pyogenic abscesses are more common in developed countries. Pyogenic abscess severity is dependent on the bacterial source and the underlying condition of the patient.
We treat the patient for both amoebic and pyogenic abscess so that we don't rely only on anti-amebic therapy and insure complete treatment of the cause.
4) Is there a way to confirm the definitive diagnosis in this patient?
Based on right hypochondriac and epigastric pain , fever
USG finding of hyperechoic mass in right lobe of liver along with other supportive investigations like leukocytosis ( suggestive of infection/inflammation) and ALP ( Alkaline phosphatase ) rise in LFT is a suggestive diagnosis of LIVER ABCESS.
Considering the following factors:
1) Age of the patient (21) - young & gender- male ,
2) Single abscess,
3) Right lobe involvement,
The abscess is most likely to be AMOEBIC LIVER ABCESS.
* Since we cannot take risk , we should however administer antibiotics also ( like in pyogenic liver abscess)
INFECTIOUS DISEASE (Mucormycosis, Ophthalmology, Otorhinolaryngology, Neurology):
24th CASE:
50/Male came with altered sensorium
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
SYMPTOMATOLOGY:
3 years back- HYPERTENTION
18/4/2021- TOOK COVID-19 VACCINATION- HIGH GRADE FEVER WITH CHILLS AND RIGOR
- RELIEVED ON MEDICATION
After 3 days- SIMILAR COMPLAINTS- NOT RELIEVED BY MEDICATION(ANTIPYRETICS)
28/04/2021-GENERALISED WEAKNESS AND FACIAL PUFFINESS AND PERI ORBITAL EDEMA- DROWSY STATE
04/05/2021-PRESENTED TO CASUALITY IN ALTERED STATE WITH FACIAL PUFFINESS AND PERIORBITAL EDEMA AND WEAKNESS OF RIGHT UPPER LIMB AND LOWER LIMB
ANATOMICAL LOCALIZATION:
First starts at upper or lower airways. Then Para nasal sinuses.
PRIMARY ETIOLOGY- IMMUNO SUPRESSION by DIABETES
Mucormycosis is a life-threatening fungal infection that occurs in immunocompromised patients. The most common predisposing risk factor for mucormycosis is diabetes mellitus. Rhino-orbito-cerebral mucormycosis is the most common form in diabetic patients and is characterized by paranasal sinusitis, ophthalmoplegia with blindness, and unilateral proptosis with cellulitis, facial pain with swelling, headache, fever, rhinitis, granular or purulent nasal discharge, nasal ulceration, epistaxis, hemiplegia or stroke, and decreased mental function. Diabetic ketoacidosis is the most common and serious acute complication of diabetic patients. We herein report 2 cases of fatal rhino-orbito-cerebral mucormycosis in a patient with diabetic ketoacidosis.
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
Inj Liposomal amphotericin B- It is a "true" liposomal formulation of amphotericin B with greatly reduced nephrotoxicity and minimal infusion-related toxicity. This broad spectrum polyene is well tolerated and effective against most invasive fungal infections.
Itraconazole- Fluconazole and voriconazole do not have reliable activity against the agents of mucormycosis, and the activity of itraconazole is primarily limited to Absidia species
Deoxycholate amphotericin B- The combination of amphotericin B and sodium deoxycholate is the formulation most used in clinical practice. The development of new agents such as amphotericin with lipid formulations, caspofungin, voriconazole and other azolic derivatives, promoted alternatives to amphotericin B deoxycholate. However, because of the high cost of these new drugs, their use is difficult in a scenario of limited resources. A few strategies have been devised to make the use of amphotericin B deoxycholate less toxic. In this review, we seek to describe the accumulated knowledge about this molecule, with focus on its use in continuous infusion, which appears to be an alternative to reduce toxicity, while maintaining its clinical efficacy.
- Me as a treating physician will follow same approach followed by the treating team
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
INFECTIOUS DISEASE (COVI 19):
As these patients are currently taking up more than 50% of our time we decided to make a separate log link here:
For this question that contains details of many of our covid 19 patients documented over this month and we would like you to:
1) Sort out these detailed patient case report logs into a single web page as a master chart
2) In the master chart classify the patient case report logs into mild, moderate severe and
3) indicate for each patient, the day of covid when their severity changed from moderate to severe or vice versa recognized primarily through increasing or decreasing oxygen requirements.
4) Indicate the sequence of specific terminal events for those who died with severe covid (for example, altered sensorium, hypotension etc).
MEDICAL EDUCATION:
Experiential learning is a very important method of Medical education and while the E logs of the students in the questions above represent partly their and their patient's experiences, reflective logging of one's own experiences is a vital tool toward competency development in medical education and research.
Question:
we would be very interested to learn about your telemedical learning experiences from our hospital as well as community patients over the last month even while locked down at home.


























Comments
Post a Comment