51years old with fever, cough and Shortness of breath
FINAL PRACTICAL - SHORT CASE
CHIEF COMPLAINTS
Fever since 10 days
Cough since 10 days
Shortness of breath since 6 days
HISTORY OF PRESENT ILLNESS:
Fever since 10 days which is high grade , with chills and rigors , intermittent ,relieving with medication.
Cough since 10 days which is productive ,mucoid in consistency,whitish ,scanty amount ,more during night times and on supine position ,non foul smelling ,non bloodstained .
Right sided chest pain - diffuse , intermittent dragging type , aggravated on cough ,non radiating not associated with sweating , palpitations.
Shortness of breath since 6 days , insidious onset , gradually progresive ,of grade 3 (MMRC scale ),not associated with wheeze , orthopnea , Paroxysmal nocturnal dyspnea, pedal edema .
pain abdomen , vomitings ,loose stools,
burning micturition.
PAST HISTORY
Patient gives history jaundice 15 days back that resolved in a week .
No history of Diabetes , Hypertension , Tuberculosis Bronchial asthma ,COPD , coronary artery disease , Cerebrovascular accident ,thyroid disease.
FAMILY HISTORY :
No relevant history
PERSONAL HISTORY:
Patient is a chronic smoker - smokes 5 cigarettes per day from past 25 years .
He is a chronic alcoholic - consumes 300 ml whisky per day ,but stopped since 3 months.
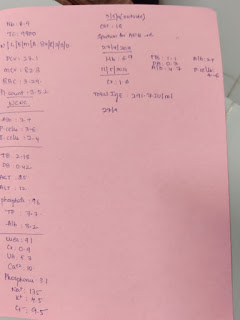
GENERAL EXAMINATION :
He is conscious, cooperative,cohorent
No signs of pallor ,cyanosis ,icterus ,koilonychia , lymphadenopathy ,edema .
Vitals :
Pulse - 84 beats / min ,normal volume ,regular rhythm,normal character ,no radio femoral delay,radio radial delay.
BP - 110/70 mmhg ,measured in supine position in both arms .
Respiratory rate -23 bpm
Inspection:-
Chest appears Bilaterally symmetrical & elliptical in shape
Respiratory movements appear to be decreased on right side
No dilated veins, scars, sinuses, visible pulsations.
Palpation:
Vocal fremitus-
Abdomen is distended.
Umbilicus is central in position.
All quadrants of abdomen are equally moving with respiration except Right upper quadrant .
No visible sinuses scars, visible pulsation engorged veins are seen
Palpation:
All inspectory findings are confirmed.
No tenderness .
Liver is palpable 4 cm below the costal margin and moving with respiration.
Spleen is not palpable.
Percussion:
Auscultation:
Inspection:
Shape of chest normal
JVP- not raised
No precordial buldge, pulsations are seen
Palpation:
Apical impulse was felt at 5th intercoastal space 1 cm medial to mid clavicular line
Auscultation:
Mitral area, tricuspid area, pulmonary area, aortic area- S1,S2 heard.
No murmurs
All higher mental functions, motor system, sensory system and cranial nerves- intact
Right sided Pleural effusion likely infectious etiology.
Hepatomegaly - ? Hepatitis or ? Chronic liver disease
Investigations :
Total count -2250 cells
Differential count -60% Lymphocyte ,40% Neutrophils
No malignant cells.
Pleural fluid protein / serum protein= 5.1/7 = 0.7
Pleural fluid LDH / serum LDH = 190/240= 0.6
Interpretation: Exudative pleural effusion.
Serum creatinine-0.8 mg/dl
CUE - normal









Comments
Post a Comment