A 40 YEAR OLD LADY WITH DYSPHAGIA, FEVER AND COUGH
A 40 year old lady who works in cotton fields came to the hospital with the chief complaints of :
- DIFFICULT IN SWALLOWING,FEVER AND COUGH, SINCE 2 MONTHS
- Fever since 2 months which is sudden in onset, intermittent and high grade (on and off associated with chills and rigor).
- Cough since 2 months on taking food and liquids which was initially non productive then associated with sputum which is white in color , moderate in quantity and non foul smelling
- difficulty in swallowing since 2 month . It was initially difficult only with solids but then followed by liquids also.
Not a K/C/O Diabetes, Hyper Tension , Asthma ,TB ,CAD.
As patient was diagnosed with RVD positive in 2012, she is on ART since 2 months (CD4-420).But on 18/05/2021, 10.45am she is TB positive.
Biomass fuel exposure - positive.
FAMILY HISTORY:
Her husband died in 2012 due to RVD. She has 2 kids with him
PERSONAL HISTORY:
Diet - mixedAppetite - normal
Sleep - inadequate (since 2 months)
Bowel and Bladder movements - regular
OBSTETRIC HISTORY:
Age of marriage - 18 yearsAge of 1st child birth - 20 years
Gravida - 2, Para - 2 (1 Caesarian section)
GENERAL EXAMINATION:
No Icterus
No Clubbing
No Lymphadenopathy
VITALS:
Temperature - Afebrile
Pulse Rate - 108bpm
Respiratory Rate - 14cpm
BP - 90/70 mm/Hg, left arm (sitting position)
SPO2 at room air - 96%
ENT EXAMINATION:(17/05/2021)
ORAL CAVITY AND OROPHARYNX:
Normal on examination
NECK EXAMINATION:
laryngeal crepitus- positive(aspiration? TE Fistula?)
SYSTEMIC EXAMINATION:
CVS:
S1 and S2 heart sounds - heard
RESPIRATORY SYSTEM:
Elliptical and bilaterally symmetrical chest
Both sides moving equally with respiration
Bilateral air entry- present
CNS:
No abnormal defectsPER ABDOMEN:
Soft and bowel sounds can be heard
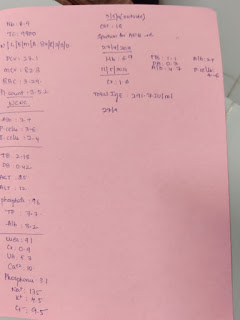
INVESTIGATIONS:
- CBP, LFT, RFT, Urine analysis
Decrease in HEMOGLOBIN, Raise in CRP.
- ECG
- BARIUM SWALLOW
- (ON 17/05/2021,12PM) OTHER INVESTIGATIONS:ENT opinion taken I/V/of dysphagia
PLAN for FLP
- ENDOSCOPY (19/05/2021):
- CECT(contrast-enhanced computed tomography),21/05/2021:
- X-ray:
- 2D ECHO:
14/05/2021:
40/female with RVD since 2 months on ART with dysphagia secondary to Esophageal Candidiasis ?Tracheoesophageal fistula ? Stricture
It can be any of the above diagnosis
TREATMENT:
RT FEEDING MILK + PROTEIN POWDER 200ml - 2nd HRLYWATER - 100ml - HRLY
TAB PANTOP 40mg RT/OD
TAB FLUCANAZOLE 100mg RT/OD
TAB DOLOTGRAVIR(50mg), LAMIVUDINE(300mg),TENOFOVIR(350mg) RT/OD
CANDID MOUTH PAINT LA
BP/RR/PR/TEMP/4th HRLY
- TPR GRAPHIC CHART
ANTI RETRO VIRAL TREATMENT:
At present there are no vaccine or cure for treatment of HIV Infections. But these ART suppress HIV infection before complications can be occur and proved to be useful in prolonging life of several ill patients.
Classification of drugs used for ART:





















Comments
Post a Comment