67yr old male with fever and shortness of breath
A 67 yr old male patient who was a daily wage labourer 5yrs back has come to the OPD with
CHIEF COMPLAINT:
fever•.• 20days
Shortness of breath •.• 10days
HOPI (18.02.2022)
patient was apparently a symptomatic 5yrs ago then his daily rotuine was
“Wakes up at 6am, complete his nature calls,brushes with neemstick, have’s his tea and takesbath , he takes rice as his breakfast and dinner, skips his lunch most of the times .spend his rest of the time with neighbours and watching tv sleeps at around 9pm”
SOB was insidious in onset, gradually progressing from grade 1 to grade.2 , relieved on taking rest associated with cough since 10days
no h/o orthopnea, PND
Fever was continuous type no aggravating factors and relieved on taking medications then he went to an hospital . He was there for 2days and the fever and cough subsided ,discharged and was at home for 2 days with decreased appetite so he was eating less or no ,later he developed fever and approched us
-as told by the attender
yesterday they noticed a palpable swelling on his left buttock
PAST HISTORY
He had an injury to the knee joint 5yrs back got surgically corrected then he was diagnosed with diabetes and hypertension . And was on regular medications .
Lifestyle modifications(?)
No h/o asthma ,TB, allergies,epilepsy
PERSONAL HISTORY
appetite- decreased
Diet-mixed
Sleep- not adequate
Bladder -regular
Bowel - no passage of stools •.•3days( since there is no food intake)
Addictions- smoking( occasionally) stoped 5 yrs ago
FAMILY History
Not significant
GENERAL EXAMINATION
patient was conscious ,coherent ,cooperative and well oriented to time ,place ,person.
Poorly built and poorly nourished
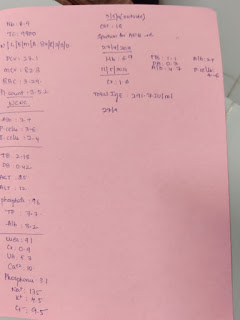
Vitals ( 20.02.2022)
RR- 20cpm
PR- 92bpm
BP-120/80mmHg
Temperature- 98*F
No pain
Pallor-present
Icterus-absent
Cyanosis absent
Clubbing absent
No Generalized Lymphadenopathy
LOCAL EXAMINATION
After taking informed consent patient was examined in sitting and supine posture in a well lit room exposing chest and abdominal area.
INSPECTION
HANDS
pallor- present
No tophi, no tremors
NAIL
Left hand
Right hand
Skin
At present it was dressed
Skin turgor
ARMS
No excoriation
No bruising
No AV fistulas
MOUTH
was unhygienic
No gingival hypertrophy
Respiratory system
Inspection:
palpation-apex beat felt in 5 th intercoastal area
Percussion. ( When patient was admitted)
Rt. Lt
supra clavicular. Resonant Rltvly dull
Infra clavicular. Resonant ”
Mammary. R. Dull Resonant
Infra mammary. R. Dull Resonant
3.03.2022- resonance can be heard at all areas when percussed
auscultation : (when patient was admitted)
Rt. Lt
supra clavicular. Normal No
Infra clavicular. Normal No
Mammary. Decreased Normal
Infra mammary. Crepitus Normal
3.03.2022 - auscultation of above areas are normal
CVS EXAMINATION
Palpation of apex beat - felt in 5th ICS medial to MCL
Auscultation of heartbeats - normal heart sounds heard in
Mitral valve area
Tricuspid valve area
Aortic valve area
Pulmonary valve area
ABDOMEN EXAMINATION
INSPECTION
No Scars
No Distention
PALPATION
No pain on Light palpation over all quadrants
Pain in right lumbar quadrant on Deep palpation
PERCUSSION
No shifting dullness
AUSCULTATION
No vascular bruits heard
INVESTIGATIONS
Doppler
CT
X-ray
ECG
USG
21.02.2022 to 1.03.2022 : all vitals are under control as he is under medication.
2.03.2022:
Pt c/c/c
PROVISIONAL DIAGNOSIS :
CKD 2° diabetic nephropathy with k/c/o hypertension and diabetes with cystic bronchiectasis
TREATMENT:
Day 1
Inj.. LASIX 40mg IV/BD
PAN 40mg
Nodisis 50mg
Orofer
Inj HAI S/c
GRBS 4th hrly
Nicardia 10mg po/bd
Day 2
Augmentin 1.2g Iv/bd
Tab azithro 500mg po/od
Inj lasix 40mgiv/bd
Tab atenolol 25mg po/od
Tab nodosis 500mg po/bd
Tab orofer po/bd
Tab shelcal ct po/od
Inj erythromycin 400iu s/c weekly once
Inj iron sucrose 100mg / 5ml in 100ml Na/iv/over 1hr during dialysis
Neb with doulin/ budecort 8th hrly
21.02.2022 to 03.03.2022
Inj Augumentin 1.2g/i.v/od
tab azitro 500mg/po/od
Inj lasix 40mg/iv/bd
T.atenolol 25mg po/od
T.Nodosis 500mg po/bd
T.orofer po/bd
T.shelcal ct po/od
Inj erythropoietin 4000 iv s/c weekly once
Inj iron sucrose (100mg/5ml) in 100ml /NS / iv over im during dialysis
Neb Budecort and Duolin - 8th hrly
Strict I/O monitoring
Elong with above medication :
24.02.2022 to 28.02.2022 - inj clindamycin 600mg/iv/tid
26.02.2022 to 28.02.2022 - tab dolo 650 mg po/qid
1.03.2022 - syp potchlor 10ml/po/ tid
2.03.2022 - fluid restriction - < 1.5 lit/day
salt restriction - < 2g/day
Tab pan 40 mg po/od
3.03.2022 - inj metogyl 500mg/tid























Comments
Post a Comment